There is an increasing tendency to want to explain everything human, from stress, to being gay, or having a zest for life as something that is 'in our genes'. The explosion of biomedical research into genetics recently has had a major impact on popular ideas about what defines a person; 'genetic thinking' has become so hugely influential that human life now seems almost determined by a person's genetic make-up.
This 'geneticisation of society' (1) also filters through to assumptions about family life. There is a tendency to think that genetic relationships are the relationships that really matter in families, whereas non-genetic relationships are less well-recognised as important, and sometimes not even seen as 'real'.
But how do genes and genetic relationships actually matter in the messy and complex world of everyday life? Is there perhaps an argument that we need to think more critically about the supposedly ever-increasing importance of genetic links?
These questions were addressed in the event 'Do Genes Matter? Families and Donor Conception ', co-organised by the Progress Educational Trust and the Morgan Centre at the University of Manchester. It drew together a panel of speakers discussing genetic connections and family life from the legal, sociological and scientific points of view.
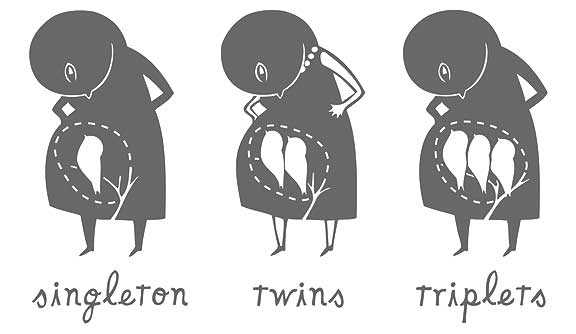
The event looked specifically at families through donor conception: families formed using donated eggs, sperm or embryos from a third party. Whereas genetic families might not have to think too hard about what genes mean to them, families by donor conception face a series of questions because they operate outside the framework that family relationships are defined by sharing genetic material. These families therefore offer an interesting viewpoint from which to explore the meaning and importance of genes.
Carol Smart, professor of sociology at the University of Manchester, presented findings from our recently finished sociological study 'Relative Strangers', which looked at how parents as well as grandparents experience the impact of donor conception on family life. She suggested that while people do think genes matter, the way in which they understand what genes are and what they do is far from straightforward. There was no consensus at all about how genes matter or why.
We also discovered that people are able to hold entirely contradictory views at the same time, saying that on the one hand, genes are important, and on the other, they don't matter at all. Smart gave the example of a grandmother who felt that it made no difference that her grandchildren were conceived using donor embryos, and yet wondered if perhaps her grandchildren's taste for olives was due to being conceived from a Spanish donor egg.
Erika Tranfield, co-founder of Pride Angel and member of the panel, suggested that parents and donors in non-clinical donor arrangements hold very different views on the meaning of the genetic relationships that ensue from donor conception, thus adding to the idea that the social meaning of genes is in fact very varied.
The idea that there is a need to question the meaning of genetic connections was taken further by Natalie Gamble of Natalie Gamble Associates. Gamble spoke of how courts of law perceive genetic relationships in families; cases involving donor conception andsurrogacy present some unique challenges to the courts, which are faced with the task of determining how to prioritise relationships. Gamble showed that in recent legal cases genes are both understood to determine relationships, and carry limited significance.
In the light of this complexity, it might be assumed that at least scientists know what genes are and what they do. However, Anneke Lucassen, professor of clinical genetics at the University of Southampton, persuasively argued that even from a scientific point of view, genes and the way they work are infinitely complex. She noted that only a very small proportion of genes can be relied upon to predict a person's characteristics.
The message that emerged with some force on the evening was that genetic connections operate with extraordinary complexity and that the social, scientific and legal meaning of genes is deeply varied and intricate. How we view them, the meaning we attach to them, and how they are understood to matter, shift and change. What emerged from the discussion was that it is important to view genetic relationships as one factor among a multitude of others shaping life and family relationships. The event thus provided a sobering perspective on the seemingly central significance of genes, suggesting that other things matter too.



 Research studies like this are often done in other countries such as the UK, Canada, and Australia. However, this one is being conducted in the US. Please help, we need more support in the US for communication information to help us be the best parents we can. They say that the survey takes about 20 minutes, but really it's more like 10 minutes. Here are the details: The Family Communication Project (FCP) is a collaborative research effort lead by Dr. Martha Rueter at University of Minnesota. The FCP team includes researchers from across the U.S. and the families who participate in FCP research studies. Working together, team members are helping to understand how to promote children’s health and well-being through family communication. If you would like to talk to Dr.Rueter to learn more about the FCP, please give a call at (612) 625-3163 or email Dr.Rueter at mrueter@umn.edu. You can also check out our website at:
Research studies like this are often done in other countries such as the UK, Canada, and Australia. However, this one is being conducted in the US. Please help, we need more support in the US for communication information to help us be the best parents we can. They say that the survey takes about 20 minutes, but really it's more like 10 minutes. Here are the details: The Family Communication Project (FCP) is a collaborative research effort lead by Dr. Martha Rueter at University of Minnesota. The FCP team includes researchers from across the U.S. and the families who participate in FCP research studies. Working together, team members are helping to understand how to promote children’s health and well-being through family communication. If you would like to talk to Dr.Rueter to learn more about the FCP, please give a call at (612) 625-3163 or email Dr.Rueter at mrueter@umn.edu. You can also check out our website at: